Nicorette® (nicotine)

Smoking continues to be the leading cause of preventable illness and premature death in England1. In 2019, 74,600 people died from smoking-related diseases, which represents 15% of all deaths3. As a result, about 50% of all lifelong smokers die prematurely, losing on average around 10 years of life1.
Smoking-related deaths⁴
35% of all deaths from respiratory diseases
|

25% of all deaths from cancer
|

12% of all deaths from circulatory diseases
|
Benefits of patients stopping smoking
In addition to the health benefits of stopping smoking for patients, there is also a positive impact:

Reducing costs to the NHS on smoking-related diseases5,6
|

Fewer visits to Healthcare Professionals (HCPs) due to better health5,6
|

Patients saving money that they would've previously spent on cigarettes5,6
|
Smoking costs the NHS approx. £2.4bn each year²
In January 2023, 14.7% of the adult population in England smoked.8 Generally, this population needs significantly more NHS resources than the non-smoker population does on average.
• In 2019/20, 506,100 hospital admissions can be attributed to smoking, which translates into 4% of all hospital admissions1
• Smokers are also a key driver of lost productivity estimated to be at £13.2bn each year due to smokers being more likely to become ill while of working age2
• Due to being more prone to sickness and long-term health implications, there is an estimated cost to the NHS of £1.2bn and an additional £1.2bn to social care each year2
• As a result, reducing smoking is a key priority for health services in England7,10 | 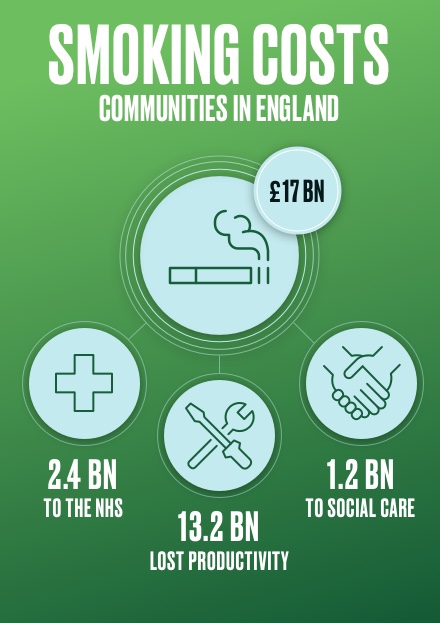 |
 | Smokers visit their GP 35% more than non-smokers¹GPs services are already in high demand9, with even more strains on it following the Covid-19 pandemic9. Smokers are visiting their GP over proportionally compared to non-smokers adding to this strain1.
Government figures show that the total costs of smoking to primary care at £1.1bn each year10. And GPs continue to be the first “port of call” for smokers when they want to quit1.
Cancer Research UK found that ending smoking could free up 75,000 GP appointments a month in England alone11.
As a matter of routine, GPs should make every contact count and identify smokers and offer smoking cessation interventions1.
|
Health inequalities and smoking
Due to smoking-related diseases, differences in smoking prevalence across the population translates into differences in death rates and illness. As smoking rates have decreased over the last 10 years, smoking has proportionately become increasingly common in more disadvantaged communities1.
Smoking is the single-largest driver of health inequalities in England12,13.
• Around 25% of people in routine and manual occupations smoked, compared with 10% in managerial and professional occupations1.
• Compared to those working, unemployed people are almost twice as likely to smoke1.
• People with a serious mental illness are over 12 times more likely to smoke compared to the national average1.
• Women in the most deprived areas are 6x more likely to smoke during pregnancy compared to those from more affluent areas7.
• Children living with parents who both smoke are nearly three times more likely to become smokers compared to children growing up in a non-smoking household.14.
• The risk of smoking dependence increases when smoking begins early15.
• Smoking is driven by nicotine dependence but, for those trying to quit, urges to resume smoking can be recurrent and persistent, even after withdrawal symptoms reduce15. It can take many attempts to quit16.
• A recent analysis from Action on Smoking and Health (ASH) Scotland found that, in 2023, the lowest-income households in Scotland will spend 29.4% of their income on tobacco. This is nine times higher than similar highest-earning households17. | 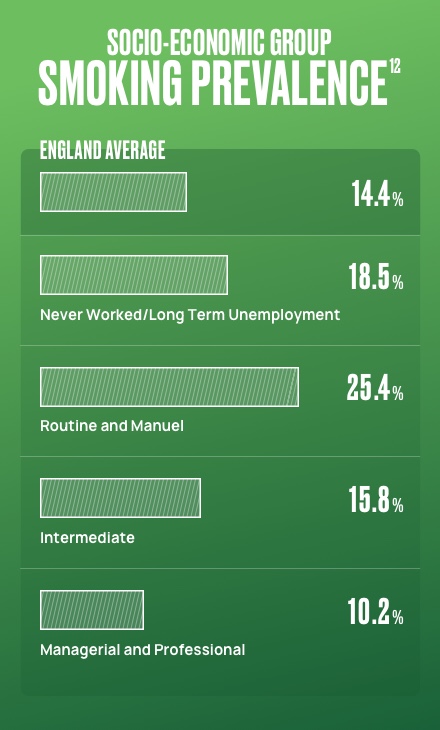 |
 | Smokers on average spend £2000 a year on cigarettes¹
Smokers in general are paying large amounts of their income on cigarettes2, especially considering that many smokers live in more disadvantaged communitites2. Around a quarter of a million children live in households where expenditure on smoking tips them below the poverty line due to expenditure on tobacco13.
Spend on cigarettes is estimated to be £12bn in England, which translates into £2,000 per smoker each year2.Depending on the number of cigarettes someone smokes, this could be much more. |
Nicotine Replacement Therapy (NRT) is a cost-effective intervention¹⁹
Any intervention to help somebody quit smoking is a cost-effective intervention, as it supports the health of the patient:
72 hours after quitting breathing may become easier and energy levels could increase20
|

2-12 weeks after quitting blood circulation could improve20
|

1 year after quitting the risk of heart attack has halved compared to a smoker20
|

10 years after quitting the risk of lung cancer falls to around 50% of that of a smoker20
|
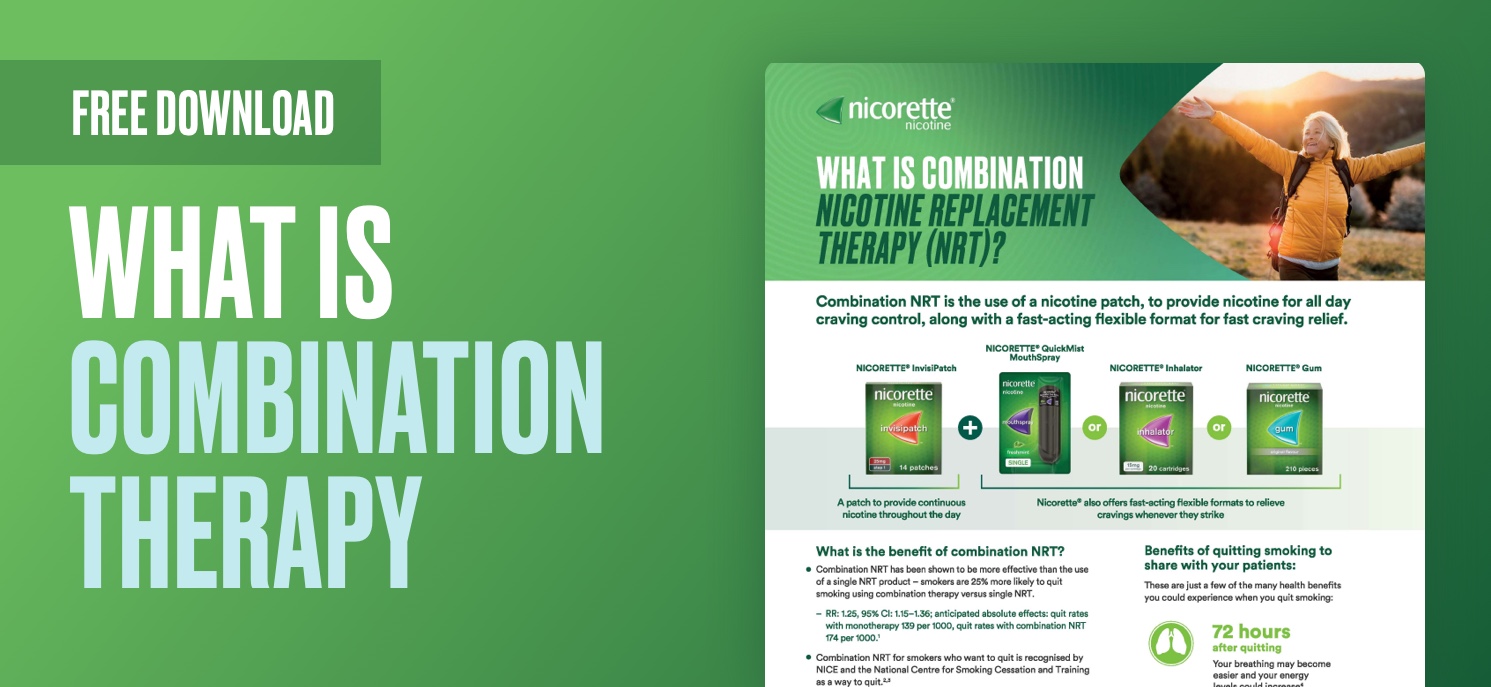
By improving the patient's health in the long term, the costs to the NHS are also reduced21. Data shows that if a patient is prescribed a combination of a long and short acting NRT, they are significantly more likely to quit compared to single NRT22.
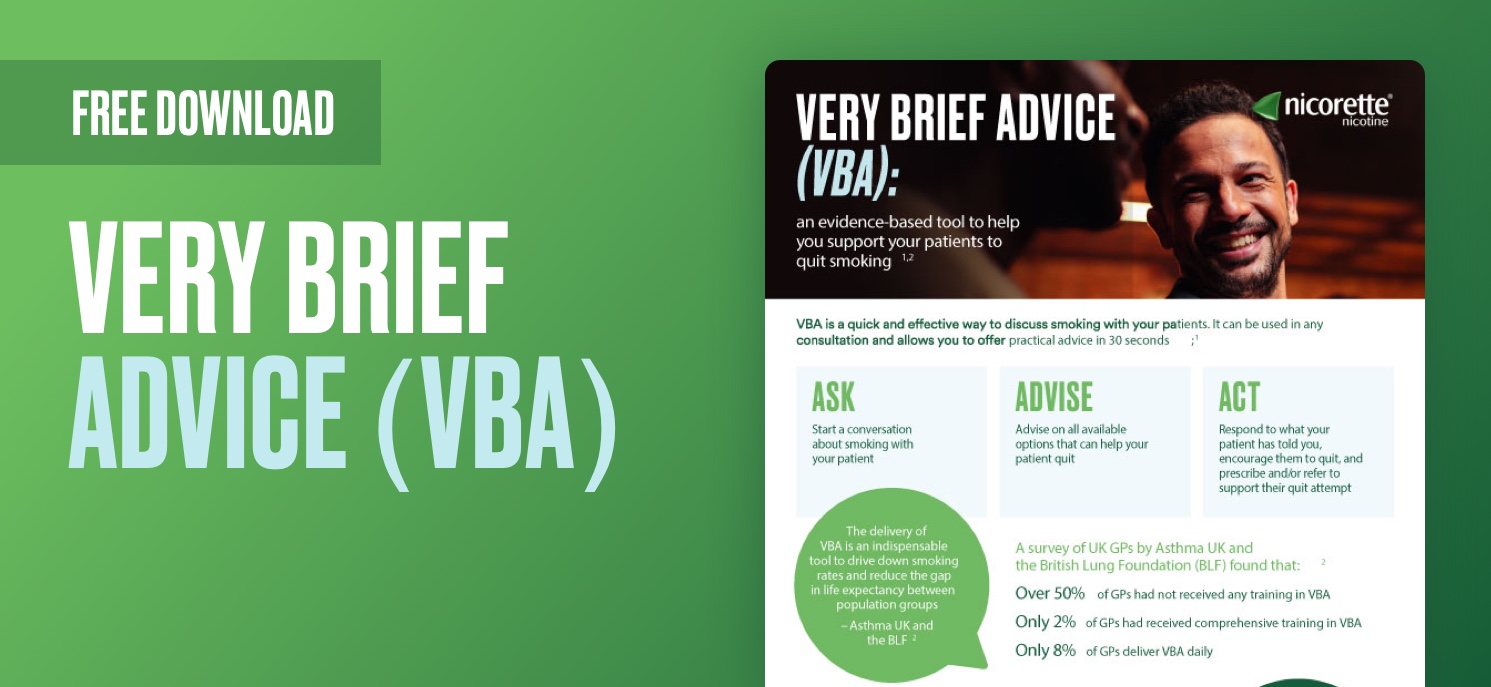
Download resources for healthcare professionals
Download resources for patients
Money saving illustration

Click here for NICORETTE® (nicotine) Prescribing Information
Adverse events should be reported. Reporting forms and information can be found at https://yellowcard.mhra.gov.uk/. Adverse events should also be reported to McNeil Products Limited on 0808 238 9999.
|
References
1. PHE Guidance, 2019. Health matters: stopping smoking – what works? Available here.
2. Action on Smoking and Health. Available here.
3. NHS. Statistics on Smoking, England, 2020. Available here.
4. NHS. Statistics on Smoking Data tables, England, 2020. Available here.
5. PHE Guidance: Tobacco commissioning support: principles and indicators Tobacco commissioning support: principles and indicators - GOV.UK (www.gov.uk)
6. PHE Guidance: Health matters: smoking and quitting in England. Available here.
7. The NHS Long term Plan. https://www.longtermplan.nhs.uk/
8. Department of Health. Smoke-free generation: tobacco control plan for England. Available here.
9. BMA. Pressures in general practice data analysis. Available here.
10. PHE. Cost of smoking to the NHS in England:2015. Available here.
11. Cancer Research UK. Ending smoking could free up 75,000 GP appointments each month. Available here.
12. Action on Smoking and Health (ASH). Health Inequalities and Smoking. Available here.
13. RCP London. Health inequalities and tobacco. Available here.
14. Loenardi-Bee J, Jere M, Britton J. Exposure to parental and sibling smoking and the risk of smoking. Thorax 2011;66(10):847-55
15. Benowitz NL. Addiction. N Eng J Med 2010;362(24):2295-2303
16. Chaiton M, Diemert L, Cohen JE, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open 2016;6:e011045. doi: 10.1136/bmjopen-2016-011045
17. ASH Scotland Calls for increased cessation support for Scotland’s poorest communities. Available here.
18. ONS RPI: Ave price – cigarettes 20 king size filter. Available here.
19. NICE Tobacco: preventing uptake, promoting quitting and treating dependence: update: Evidence review for cessation and harm reduction treatments https://www.nice.org.uk/guidance/ng209/evidence/k-cessation-and-harmreduction-treatments-pdf-10890777861
20. NHS Better Health. Quit Smoking. https://www.nhs.uk/better-health/quit-smoking/
21. Evison M, Cox J, Howle F, et alHealth economic analysis for the ‘CURE Project’ pilot: a hospital-based tobacco dependency treatment service in Greater Manchester. BMJ Open Respiratory Research 2021;8:e001105. doi: 10.1136/bmjresp-2021-001105
22. Lindson N, Chepkin SC, Ye W, Fanshawe TR, Bullen C, Hartmann‐Boyce J. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database of Systematic Reviews 2019, Issue 4. Art. No.: CD013308. DOI: 10.1002/14651858.CD013308
Date of preparation: Apr 2023