
Eczema is a common skin problem that can affect people of all ages, especially children. In fact, research has shown that one in five children suffer from eczema compared to one in 10 adults1.
Despite being a long-term, chronic condition, some children can outgrow their eczema. But it can also be managed through the regular application of emollients to restore the skin barrier2. However, there can be a psychological and emotional impact on people who suffer with eczema3.
In this guide, we will give you all the information you need to know about eczema – the causes, how it presents, and how best to give advice on managing eczema.
Quick links
What is eczema?
Eczema, also known as dermatitis, is a type of chronic inflammatory skin condition that compromises the skin barrier4. This leads to dry, cracked and itchy skin, as well as redness, soreness and inflammation4.
It is non-contagious and episodic in nature4. Sufferers typically experience periods of flare-ups, when the skin is red and itchy, as well as periods of remission – when the skin is relatively calm but may still be dry and sensitive4.
Eczema is usually the result of a compromised skin barrier, which struggles to retain moisture or protect lower layers of the skin from allergens4. However, this in turn can further damage the skin barrier, resulting in the chronic symptoms of eczema5.
What are the main types of eczema?
There are a few different types of eczema – each with their own set of symptoms4.

Atopic eczema
The most common type of eczema, atopic eczema normally presents in children before their first birthday but may also flare up in later life4. “Atopy” refers to the genetic tendency to develop allergic conditions, including those that are part of the atopic triad: atopic eczema, allergic rhinitis and asthma.
It might be the case that someone who suffers from atopic eczema also suffers from one of the other conditions in the atopic triad4.

Discoid eczema
Discoid eczema is a chronic skin condition that can cause redness, itching, and even cracking in oval patches on the patient’s skin. It most commonly appears in men aged between 50-70 and young women in their teens to 20s. Normally, a sufferer of discoid eczema will also suffer from atopic eczema6.

Varicose eczema
This is a long-term condition that usually occurs on the lower legs and presents alongside varicose veins – especially in older women7. Those who have a history of deep vein thrombosis (DVT) or obesity are more likely to develop this type of eczema7.

Dyshidrotic eczema
This is a long-term condition that usually presents with small, itchy blisters on the hands and feet. Also known as pompholyx, the symptoms of this type of eczema usually appear in two-to-three-week cycles8.

Seborrhoeic eczema
This type of eczema usually develops on the scalp and face. It’s mostly recognised by its red, scaly patch-like appearance4.

Contact dermatitis
Contact dermatitis is a type of eczema that is triggered by contact with an external irritant or allergen. This can include things like soaps, solvents and detergents9. It can clear up quickly once the substance causing the eczema symptoms has been identified9.
What causes eczema?
The exact cause of eczema is unknown, meaning that we often treat the symptoms of the condition instead. However, there are a few factors that we believe to be involved4.

Genetics
In the case of atopic eczema, we know that there is a strong genetic link between conditions associated with atopy. Recent clinical research has shown evidence that this genetic link could be a result of a missing protein in the skin, negatively affecting the strength of the skin barrier10.
Inappropriate treatment
Eczema flare-ups can also be caused by improper products that may further aggravate the skin, allowing irritants and bacteria to pass through the barrier. In turn, this triggers an inflammatory response, leading to redness, itchiness and the typical symptoms of an eczema flare-up10.
Environmental factors
Some eczema sufferers may know they have specific triggers for a flare-up, such as different foods, contact with animals, unsuitable cleansing agents like soaps and detergents, getting either too hot or too cold, and stress. All of these external factors can trigger flare-ups among customers, so it’s important that they identify and avoid these triggers.
Eczema symptoms: what to look out for
Eczema generally results in dryness and inflammation. However, this can look different depending on a person’s skin tone. For example, while this inflammation will often appear red on lighter skin tones, it might present as dark brown, purple or grey on darker skin, making it more difficult to spot11. It may also lead to hyper or hypo pigmentation – darkening or lightening of the skin.
On paler skin, eczema will usually present on the inside of the elbow or behind the knee, whereas it may appear on the outside of joints on people with darker skin.
The difference in how eczema presents on different skin tones may lead to an underdiagnosis of eczema in people of colour11.
How to manage eczema
Eczema is an incurable chronic condition. However, it can be managed through a wide variety of treatments available to help manage the symptoms4. These work by helping to rebuild the skin barrier and reducing inflammation when it flares.
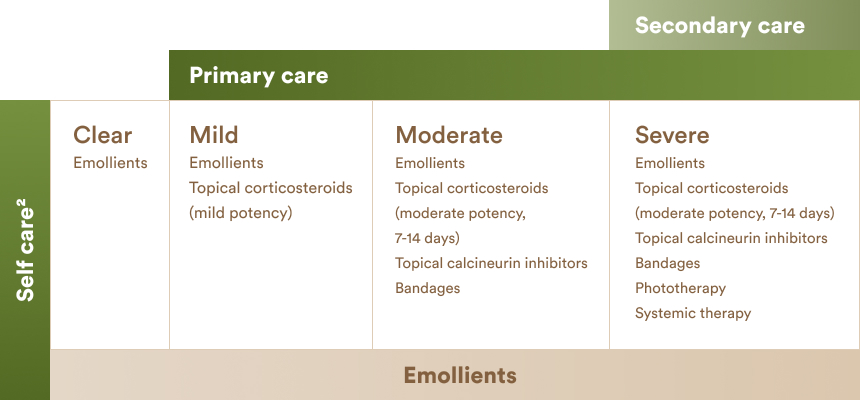
The National Institute for Health and Care Excellence (NICE) recommends a stepped approach for managing eczema symptoms, depending on the severity of the condition at the time2. Here’s an outline of the approach2.
- Tailor routine to eczema severity.
- Use emollients to manage the eczema – even when the skin is clear.
- Provide advice for customers on how to spot flare ups, so they can adjust their treatment
- Recommend your customer see a GP if appropriate.
You should refer to a GP if your customer is experiencing any of the following12:
- Skin is hot to touch
- Fever
- Signs of infection – such as oozing, crusting or redness spreading
- Flare-up is unmanageable after topical corticosteroid treatment
- Eczema is affecting their quality of life – unable to sleep from intense itching
- Causing emotional distress.
What should you use to manage eczema?

Emollients are key to properly managing eczema, during both flare ups and periods of remission2. This is because they provide a layer of oil on the skin to help slow water loss, improve hydration and prevent external irritants from entering the skin barrier13.
But not all emollients suit all people. So, healthcare professionals should provide a range of products for topical application. After all, patient preference is key to consistent emollient use2.
Apart from emollients, more moderate and severe cases of eczema may call for other products. Take a look at the different levels and the types of products recommended by NICE in the chart below.
When should you use emollients?
Emollients should be applied both during flare ups and when the skin is clear2. It’s recommended that emollients are applied liberally, 2-3 times a day to cover any dry and inflamed areas14. But bear in mind this may vary based on the size of the person, the severity of their eczema and the extent of skin dryness14.
Explore dry skin and the role of emollients
Help your customers take care of their skin with our training on dry skin and the role of emollients.
References
- National Eczema Society. Available at: https://eczema.org/information-and-advice/
- NICE (2007), Management of atopic eczema in children from birth up to the age of 12 years, National Collaborating Centre for Women’s and Children’s Health.
- Lewis-Jones S. Quality of life and childhood atopic dermatitis: the misery of living with childhood eczema, 2006, Department of Dermatology at Ninewells Hospital, Dundee, vol (8):984-92.
- NHS. Atopic eczema. Available at: https://www.nhs.uk/conditions/atopic-eczema/.
- Atopic dermatitis epidemiology and unmet need in United Kingdom M J Cork, S G Danby, G S Ogg J Dermatolog Treat 2020; 31(8) 801-809/.
- NHS Inform. Discoid eczema. Available at: https://www.nhsinform.scot/illnesses-and-conditions/skin-hair-and-nails/discoid-eczema.
- NHS. Varicose eczema. Available at: https://www.nhs.uk/conditions/varicose-eczema/.
- NHS. Pompholyx (dyshidrotic eczema). Available at: https://www.nhs.uk/conditions/pompholyx/.
- NHS. Contact dermatitis. Available at: https://www.nhs.uk/conditions/contact-dermatitis/.
- Atopic dermatitis and filaggrin. B Cabanillas, N Novak, Current Opinion in Immunology. Vol 42 Oct 2016.
- Eczema on Black Skin: What to know. Medical News Today.
- NHS. Complications Atopic eczema. Available at: https://www.nhs.uk/conditions/atopic-eczema/complications.
- Emollients and moisturisers. Available at: http://dermnetnz.org/treatments/emollients.html.
- SIGN guidelines on Atopic Eczema (2011). Management of atopic eczema in primary care. (SIGN Guideline No 125).

